

岭南现代临床外科 ›› 2020, Vol. 20 ›› Issue (02): 184-187.DOI: 10.3969/j.issn.1009-976X.2020.02.011
摘要:
老年急性胆囊炎(AC)具有起病急、急诊手术困难、病情进展快等特点,稍有不慎,即可损伤肝功能,引起弥漫性腹膜炎、胆囊坏疽穿孔等严重并发症,甚至死亡[1]。既往文献显示,针对轻中度AC患者,推荐施行早期腹腔镜胆囊切除术(LC),重度AC患者,推荐先行胃肠减压、经皮肝胆囊穿刺引流(PTGD)等保守治疗,后进行延期手术[2]。LC治疗AC效果已得到临床证实,但随微创技术发展与完善,经脐单孔腹腔镜胆囊切除术(TUSLC)受到临床重视,与传统LC比较,更加微创及美观,但勉强施行TUSLC可增加手术风险,引起胆道损伤、出血等一系列并发症,中转开腹手术概率较高[3]。PTGD有效解决胆囊胆汁引流问题,待炎症消退后施行TUSLC,可减少并发症,提高手术安全性[4]。在此背景下,本研究将PTGD术后择期TUSLC应用于老年AC患者,取得满意效果。
选取我院80例老年AC患者(2017年12月~2018年12月),根据手术方案分为对照组(n=40)和观察组(n=40)。2组性别、年龄、体质量指数(BMI)、腹痛持续时间、基础疾病、白细胞计数(WBC)、谷氨酸氨基转移酶(ALT)、天门冬氨酸氨基转移酶(AST)资料均衡可比(P>0.05),且研究征得我院伦理委员会审核批准。见表1。
表1 两组临床资料对比
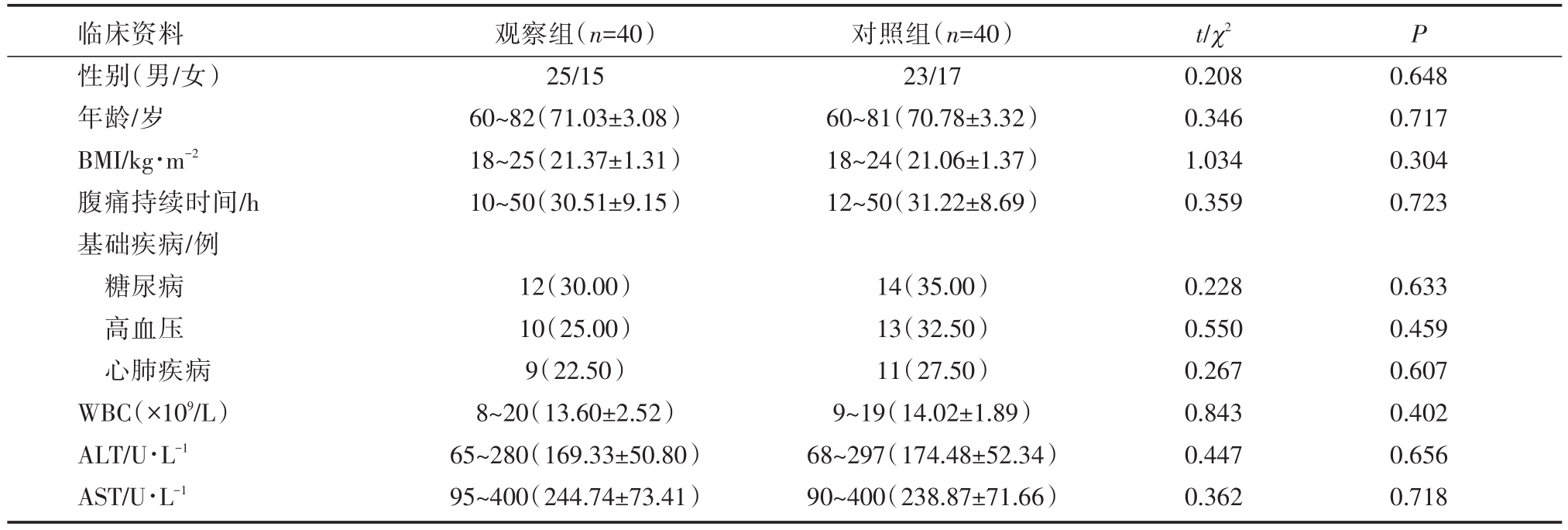
临床资料性别(男/女)年龄/岁BMI/kg·m-2腹痛持续时间/h基础疾病/例糖尿病高血压心肺疾病WBC(×109/L)ALT/U·L-1 AST/U·L-1观察组(n=40)25/15 60~82(71.03±3.08)18~25(21.37±1.31)10~50(30.51±9.15)对照组(n=40)23/17 60~81(70.78±3.32)18~24(21.06±1.37)12~50(31.22±8.69)t/χ2 0.208 0.346 1.034 0.359 P 0.648 0.717 0.304 0.723 12(30.00)10(25.00)9(22.50)8~20(13.60±2.52)65~280(169.33±50.80)95~400(244.74±73.41)14(35.00)13(32.50)11(27.50)9~19(14.02±1.89)68~297(174.48±52.34)90~400(238.87±71.66)0.228 0.550 0.267 0.843 0.447 0.362 0.633 0.459 0.607 0.402 0.656 0.718
入组标准符合AC诊断标准[5];B超、CT等影像学检查确诊;发病至入院时间≤3 d;年龄≥60岁;患者及家属知晓并签署同意书。排除标准包括手术禁忌证者;严重心脑血管疾病者;凝血障碍者;腹部手术史者;出血倾向者;其他胆囊疾病者;临床资料不完整,无法完成研究者。
2组接受补液、胃肠减压、禁食等治疗。观察组施行PTGD,术前肌肉注射哌替啶50 mg,左侧卧位,根据B超检查结果确定穿刺点、方向、深度,利多卡因(浓度为2%)局麻,自右侧腋前线取一切口,长度约0.2 cm,B超引导下,8 F猪尾形穿刺引流管插入胆囊,拔出针芯,固定引流管,接通引流装置,无菌敷料包扎。术后密切观察患者腹部体征、生命体征,并予以营养支持、抑酸、抗感染等对症治疗。PTGD术后2~4个月内行TUSLC,气管插管全麻,拔除PTGD引流管,自脐上缘正中处作一纵向切口,长度约1.5 cm,逐级分离皮肤,直至进入腹腔,置放单孔三通道装置,开放人工气腹,压力维持在14 mmHg,于三通道装置放入操作器械、腹腔镜,腹腔镜引导下,分离胆囊三角区,游离胆囊管、胆囊动脉并切断,切除胆囊,彻底止血,退镜取胆囊,闭合切口。对照组施行PTGD+传统腹腔镜胆囊切除术(LC),PTGD操作步骤如观察组,LC操作步骤为,气管插管全麻,平卧位,气腹针穿刺进入腹腔,建立人工通道,常规三孔法放入操作器械、腹腔镜,观察胆囊壁和局部组织有无粘连,出现粘连者,先行分离,游离胆囊三角,离断胆囊管、胆囊动脉,剥离胆囊,电凝止血,生理盐水反复冲洗,取出胆囊,缝合切口。
2组手术时间、胃肠功能恢复时间、术中出血量、白细胞恢复时间、住院时间;2组术后1 d、3 d、7 d疼痛程度。应用视觉模拟评分法(VAS)评估,最高分10分,分值越低疼痛程度越轻。2组并发症。
通过SPSS 23.0处理,计量资料以x±s表示,两组间计量资料使用t检验,计数资料以n(%)表示,行χ2检验,P<0.05为差异有统计学意义。
观察组白细胞恢复时间、住院时间、胃肠功能恢复时间短于对照组,术中出血量少于对照组(P<0.05),2组手术时间比较,差异无统计学意义(P>0.05)。见表2。
术后1 d、3 d、7 d观察组VAS评分较对照组低(P<0.05)。见表3。
观察组并发症发生率5.00%较对照组22.50%低(P<0.05)。见表4。
表2 围术期指标(x±s)
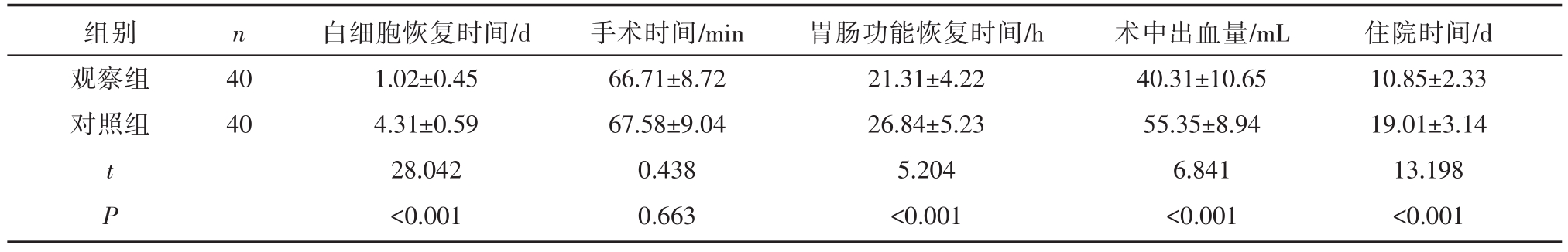
组别观察组对照组n 40 40 t P白细胞恢复时间/d 1.02±0.45 4.31±0.59 28.042<0.001手术时间/min 66.71±8.72 67.58±9.04 0.438 0.663胃肠功能恢复时间/h 21.31±4.22 26.84±5.23 5.204<0.001术中出血量/mL 40.31±10.65 55.35±8.94 6.841<0.001住院时间/d 10.85±2.33 19.01±3.14 13.198<0.001
表3 VAS评分(x±s,分)
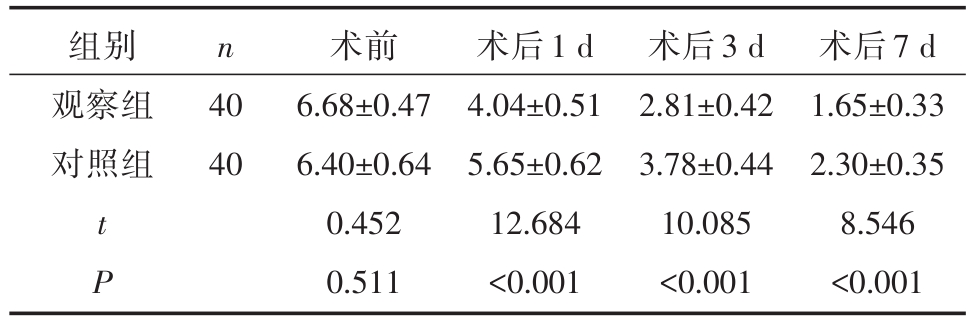
组别观察组对照组n 40 40 t P术前6.68±0.47 6.40±0.64 0.452 0.511术后1 d 4.04±0.51 5.65±0.62 12.684<0.001术后3 d 2.81±0.42 3.78±0.44 10.085<0.001术后7 d 1.65±0.33 2.30±0.35 8.546<0.001
表4 并发症[n(%)]

组别观察组对照组n 40 40肝脏损伤0(0.00)1(2.50)气胸1(2.50)3(7.50)胆漏0(0.00)2(5.00)肠穿孔1(2.50)3(7.50)χ2 P总发生率2(5.00)9(22.50)5.165 0.023
随社会老龄化趋势日益明显,老年急性胆囊炎(acute cholecystitis,AC)发病率呈逐渐升高趋势,据统计,AC在年龄≥70岁人群中发病率达50%,若未及时治疗,可在短期内出现严重并发症,危及其生命安全[6]。因此,老年AC患者的早期治疗显得十分重要。
PTGD可通过穿刺置管引流脓性胆汁,缓解胆囊管梗阻,降低胆囊压力,抑制毒素吸收,缓解炎性症状,为择期手术治疗提供良好基础[7]。LC是临床治疗老年AC重要手段,能有效清除胆囊病变,控制患者临床症状及体征,但其存在切口大且多、美观性不足等问题。TUSLC是在LC基础上改良而来,由于脐为机体自然瘢痕,自脐上缘入路,手术切口更为隐蔽,能满足患者对美观需求[8]。研究显示,PTGD联合TUSLC可改善AC患者围术期指标,降低中转其他手术风险[9]。Lin等[9]总结752例老年急性结石性胆囊炎实施经皮胆囊造口置管引流术(PC)+腹腔镜胆囊切除术(DLC),结果显示出PC+DLC较单纯LC具有术中出血少、胆管损伤率低、残余结石和胃肠器官损伤率低的优势;同时DLC组患者ICU入院和死亡的发生率较低,重复手术的发生率明显较低。然而,PC+DLC总住院时间明显延长,治疗成本明显高与LC组患者。Ke等[10]总结急性胆囊炎患者经皮经肝胆囊引流术(PTGBD)后的紧急胆囊切除术(EC)和延迟胆囊切除术(DC)的效果,结果为在中度(Ⅱ级)急性胆囊炎患者中,PTGBD和EC对胆囊炎有很高的疗效;PTGBD后DC患者预后较好,OC发生率较低,术中出血少,术后腹腔引流时间短,胆囊切除术后住院时间短,呼吸衰竭发生率较低,ICU入院次数较EC少,胆囊病理过程逆转。PTGBD+DC组术后住院时间较长。
本研究数据显示,观察组白细胞恢复时间、住院时间、胃肠功能恢复时间、术中出血量优于对照组(P<0.05),与上述研究观点相符。分析原因与以下2方面有关,一方面是TUSLC手术创伤小,另一方面是PTGD术后2~4个月内施行TUSLC,此时胆囊炎症明显缓解,局部粘连减轻,手术操作相对容易,围术期指标改善更为明显[11,12]。进一步研究发现,术后1 d、3 d、7 d观察组VAS评分低于对照组(P<0.05),分析原因可能与TUSLC手术切口小有关,可减轻周围组织损伤,缓解术后疼痛,加快术后恢复。但TUSLC存在问题,即操作器械及腹腔镜置入位置集中,空间狭小,操作时存在相互干扰情况,对术者及操作者要求较高,需默契配合才能很好完成手术。
综上,PTGD术后择期行TUSLC,有助于减少老年AC患者术中出血量,缓解术后疼痛,降低并发症发生风险,缩短康复进程。
[1] Loozen CS,Oor JE,van Ramshorst B,et al.Conservative treatment of acute cholecystitis:a systematic review and pooled analysis[J].Surg Endosc,2017,31(2):504-515.
[2] 陈春华,杨林华,王坚,等.B超引导经皮经肝胆囊穿刺引流术在高危患者中的应用价值[J].肝胆胰外科杂志,2015,27(3):228-230.
[3] 林泽伟,刘晓平,刘吉奎,熊沛.腹腔镜胆囊切除术所致胆管损伤的诊治体会[J]. 岭南现代临床外科,2012,12(6):421-423.
[4] Ni QQ,Chen DB,Xu R,Shang D.The efficacy of percutaneous transhepatic gallbladder drainage on acute cholecystitis in high-risk elderly patients based on the tokyo guidelines:a retrospective case-control study[J].Medicine(Baltimore),2015,94(34):e1442.
[5] Pisano M,Ceresoli M,Cimbanassi S,et al.2017 WSES and SICG guidelines on acute calcolous cholecystitis in elderly population[J].World J Emerg Surg,2019,14:10.
[6] Escartín A,González M,Cuello E,et al.Acute Cholecystitis in Very Elderly Patients:Disease Management,Outcomes,and Risk Factors for Complications[J].Surg Res Pract,2019,2019:9709242.
[7] Hu YR,Pan JH,Tong XC,et al.Efficacy and safety of B-mode ultrasound-guided percutaneous transhepatic gallbladder drainage combined with laparoscopic cholecystectomy for acute cholecystitis in elderly and high-risk patients[J].BMC Gastroenterol,2015,15:81.
[8] Vaccari S,Lauro A,Cervellera M,et al.Cholecystectomy for acute cholecystitis in octogenarians:impact of advanced age on postoperative outcome[J].Minerva Chir,2019,74(4):289-296.
[9] Lin D,Wu S,Fan Y,Ke C.Comparison of laparoscopic cholecystectomy and delayed laparoscopic cholecystectomy in aged acute calculous cholecystitis:a cohort study[J].Surg Endosc,2019.doi:10.1007/s00464-019-07091-4.[Epub ahead of print]
[10] Ke CW,Wu SD.Comparison of emergency cholecystectomy with delayed cholecystectomy after percutaneous transhepatic gallbladder drainage in patients with moderate acute cholecystitis[J].J Laparoendosc Adv Surg Tech A,2018,28(6):705-712.
[12] 尹飞飞,李学民,段希斌,等.日间经脐单孔腹腔镜胆囊切除术65例单中心临床疗效分析[J].中国普通外科杂志,2019,34(8):712-713.
Efficacy and safety of selective transumbilical single-port laparoscopic cholecystectomy for elderly patients with acute cholecystitis after percutaneous hepatic and gallbladder puncture and drainage
中图分类号: